Harriet Blannin-Ferguson @the.breast.help is a registered midwife and an Internationally Board Certified Lactation Consultant (IBCLC). Harriet shares her insights and an overview of caesarean section recovery below.
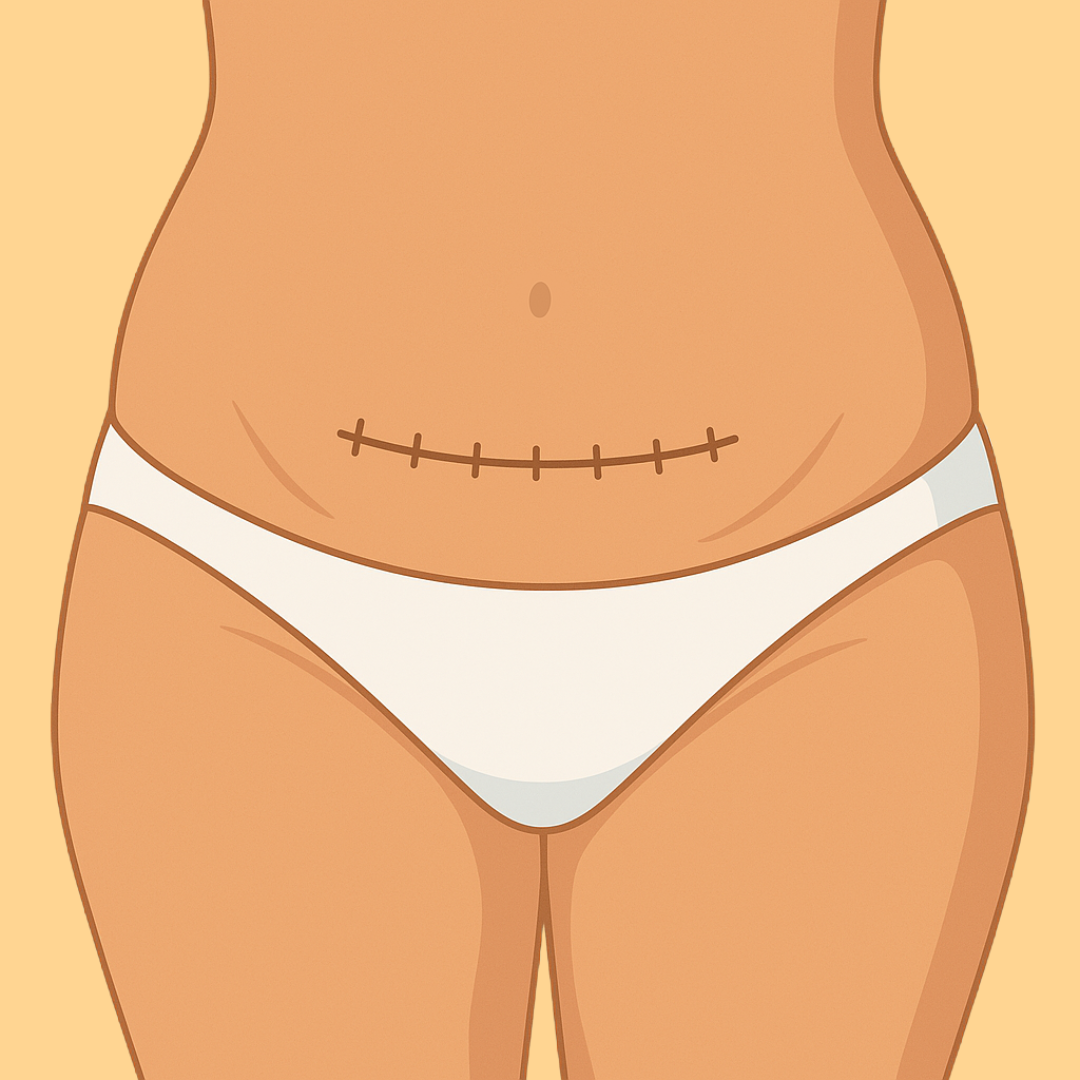
Recovering from a Caesarean birth takes time. Here’s what to expect and how to best care for yourself in the first days, weeks and months.
Hospital Stay: First Few Days
• Typical Stay: 3–5 days in hospital
• Medications: Regular pain relief medication (dependant on your level of pain) is provided alongside blood thinning medication to prevent blood clots
• Mobility: Walking within 12–24 hours is encouraged to help prevent blood clots (You’ll also be encouraged to wear compression stockings for this same reason!)
• Catheter removed: Once mobility improves
• Bleeding: Lochia (post-birth bleeding) can last up to 4–6 weeks
• Breastfeeding: Midwives can assist with positioning to reduce wound discomfort
• Leaving hospital: You will receive pain relief advice and a planned midwife check-up at home if birthing in the public system.
First 2 Weeks: Home Recovery
Do:
• Take pain relief as needed
• Keep your wound clean and dry
• Walk gently each day
• Ask for and accept help from family or friends
Avoid:
• Lifting anything heavier than your baby
• Driving (usually not before six weeks - check with your insurer and care provider for your individual situation)
• Straining your core (no crunches, planks, or heavy lifting)
• Watch for signs of infection: redness, swelling, pus, fever or increasing pain around the scar.
Weeks 3 - 6: Strength & Healing
• Pain improves – Many switch to paracetamol or ibuprofen only
• Scar care – Gentle scar massage can begin after six weeks if fully healed
• Light movement – Walking and pelvic floor exercises are safe
• GP check-up at six weeks – Clears you for driving, work, and light exercise
• Now is a good time to book in with a women’s health physiotherapist for your physical aftercare if desired.
3 - 6 Months: Feeling Stronger
• Most feel physically recovered around three months
• Core and pelvic floor rehabilitation – A women’s health physiotherapist can help (Medicare rebates may apply)
• Emotional recovery – Seek support if needed
When to Call a Doctor
• Signs of infection: fever, worsening pain, pus at the scar
• Heavy bleeding: soaking a pad in one hour or passing large clots
• Swelling: in one leg, chest pain, or breathlessness – Possible blood clot
• Emotional distress: If feeling low, anxious, or struggling with daily life, speak with a GP or support service
Support Services in Australia
• Maternal & Child Health Nurse – Free baby and maternal check-ups
• PANDA (1300 726 306) – Mental health support
• Lactation Support – IBCLC or public hospital services
• Women’s Health Physiotherapy – For pelvic floor and core recovery (GP referral recommended)
Recovery takes time. Focus on small improvements each day and seek support when needed.
Cart is Empty
Your Cart is Empty
- Choosing a selection results in a full page refresh.
- Opens in a new window.